There continues to be a great deal of public debate regarding the extent to which psychiatric medications are overused or underused in children and adolescents. One complication to answering this question well has been the difficulty getting good nationally representative numbers regarding the number of youth who take various classes of medications. This new study addresses the issue by trying to calculate reliable national estimates of medication usage and then comparing those numbers to known rates of disorders that have been found in epidemiological studies.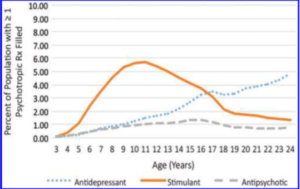
The data come from a large databases of prescribing claims from all payer sources which in sum examined over 6 million prescriptions for individuals between the ages of 3 and 24. In addition to the medication itself, a few other variables such as prescriber specialty as well as patient age and sex were also gathered. By combining these data with another large database, the authors were able to estimate the percentage of youth taking different classes of medication for the entire U.S. population during a single year.
Overall, the percentage of youth taking either a stimulant, antidepressant, or antipsychotic medication for the 2-5, 6-12, 13-18, and 19-24 age groups was 0.8, 5.4, 7.7, and 6.0 respectively. As might be expected, different age trends were observed for different types of medications with stimulants tending to peak around age 11 and antidepressants rates rising with age. Psychiatrists and child psychiatrists wrote for the most antidepressant and antipsychotic prescriptions while pediatricians were the most common prescribers of stimulant prescriptions among individuals 18-year-old and younger.
In comparing these numbers with calculated rates of different disorders from epidemiological studies, the authors find that the rate of stimulant prescriptions were well below estimates rates of ADHD while the rate of antidepressant prescriptions were well below the epidemiological rates of mood and anxiety disorders, thus suggesting that, at least when looking at the raw numbers, there was not evidence of systematic over-prescribing. The picture with antipsychotics was more difficult to interpret given the number of off-label uses for this class of medications, such as physical aggression.
The authors concluded that medications usage for stimulants and antidepressants tend to follow known epidemiological patterns for the disorders they treat. While these data offered some reassurance that medications were not being prescribed at levels that were beyond the known rates of the disorders they are designed to treat, there are of course some factors that limit a firmer conclusion. For example, some medications that are commonly used such as guanfacine were not included in this analysis. Perhaps most importantly, the study also is not equipped to assess whether or not a particular medication was appropriate for an individual patient, especially given the fact that medications for things like anxiety disorders are generally not considered to be first-line treatment.
For these reasons and others, this study is unlikely to change to minds of skeptics who have noted that the article was published in the Journal of Child and Adolescent Psychopharmacology by some authors with disclosed ties to pharmaceutical companies. Some also just reject the science regarding the rates of diagnoses as well. My own view is that over-treatment and under-treatment are not mutually exclusive categories and both are problems clinicians should try to avoid through careful assessment and judicious use of both pharmacological and non-pharmacological interventions.
Reference
Sultan RS, Correll CU, et al. National Patterns of Commonly Prescribed Psychotropic Medications to Young People. J Child Adolesc Psychopharmacology 2017, epub ahead of print.

